Hello Reader!
Welcome to the blog page of Dr. Soumya Dash, the best infertility specialist in Bhubaneswar.
Thyroid disorders are common during pregnancy and, if left unmanaged, can impact both mother and baby. Hormonal changes in the body influence thyroid function, making it essential to monitor and control thyroid function during pregnancy. As the Best Infertility Specialist in Bhubaneswar, I have encountered numerous cases where early intervention and proper management have helped ensure a safe and healthy pregnancy.
In this blog, we will discuss what thyroid issues can occur during pregnancy, their effects, and most importantly, how to control the thyroid during pregnancy effectively.

Understanding Thyroid During Pregnancy
The thyroid is a small, butterfly-shaped gland located in the neck that produces hormones regulating metabolism. During pregnancy, your body needs more thyroid hormones to support fetal development, especially in the first trimester. There are mainly two types of thyroid disorders:
- Hypothyroidism (underactive thyroid): Commonly caused by Hashimoto’s thyroiditis.
- Hyperthyroidism (overactive thyroid): Often associated with Graves’ disease.
When it comes to managing thyroid during pregnancy, early detection and treatment are crucial. Regular screening can prevent complications such as miscarriage, preeclampsia, preterm birth, and developmental issues in the baby.
Symptoms of Thyroid Disorders in Pregnancy
Recognizing the signs of thyroid imbalance can help in timely diagnosis. Here are some common symptoms:
Hypothyroidism Symptoms:
- Fatigue
- Constipation
- Cold intolerance
- Dry skin
- Depression
- Weight gain
Hyperthyroidism Symptoms:
- Increased heart rate
- Anxiety
- Excessive sweating
- Weight loss
- Tremors
- Insomnia
If you notice any of these symptoms, consult the Best Infertility Specialist in Bhubaneswar for proper screening and diagnosis.

Why Thyroid Control Is Crucial During Pregnancy
An uncontrolled thyroid during pregnancy can lead to:
- Miscarriage or stillbirth
- Poor fetal growth
- Low birth weight
- Preterm labor
- Developmental delays in the child
As the Best Infertility Specialist in Bhubaneswar, I recommend that every pregnant woman have their thyroid function tested early in pregnancy or even before conception if they have a history of thyroid disorders.

How does the thyroid gland during pregnancy impact fetal brain development?
The thyroid gland during pregnancy plays a fundamental role in fetal brain development, especially during the first trimester when the fetus is entirely dependent on maternal thyroid hormones for neurodevelopment. Adequate maternal thyroid hormone levels—primarily thyroxine (T4)—are critical for processes such as neural cell proliferation, cortical development, neuronal migration, and overall brain architecture.
Key impacts of the thyroid during pregnancy on fetal brain development include:
- Impaired Cognitive and Motor Development: Maternal hypothyroidism (low thyroid hormone) during pregnancy, even in mild or subclinical cases, is associated with lower IQ, delayed neurological maturation, and psychomotor impairments in the child. The adverse effects of thyroid hormone deficiency can be irreversible, particularly if not corrected early in gestation.
- Reduced Brain Volume: Both low and high maternal thyroid function are linked to smaller total grey matter and cortical volume in children, highlighting the importance of balanced thyroid levels.
- Risk of Neurodevelopmental Disorders: Children born to mothers with thyroid disorders during pregnancy show higher incidences of developmental delays, learning disabilities, and may also display an increased frequency of behavioral issues such as ADHD-like symptoms.
- Critical Time Window: The most vulnerable period is early gestation, before the fetal thyroid becomes functional (around 12–14 weeks). During this period, the maternal supply of thyroid hormone is essential for proper cortical and neurological development.
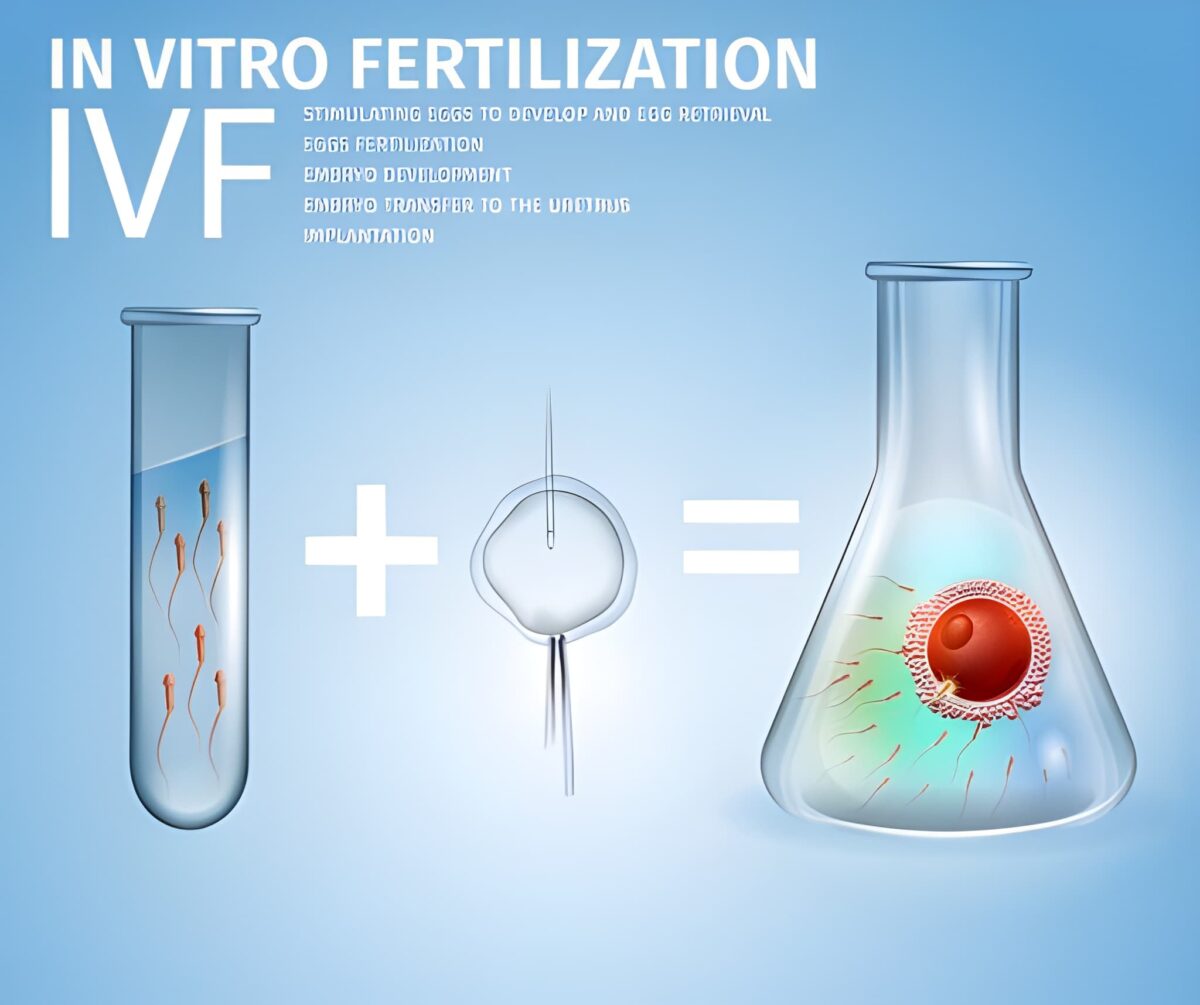
Also Read: Preparations needed before starting IVF

What are the risks of an uncontrolled thyroid during pregnancy?
Uncontrolled thyroid during pregnancy in Bhubaneswar, as in other places, poses significant risks to both mother and baby. Key complications from unmanaged thyroid disorders (hypothyroidism or hyperthyroidism) during pregnancy include:
- Miscarriage and stillbirth: Untreated thyroid imbalances increase the risk of pregnancy loss.
- Preterm birth: Babies may be born before 37 weeks, which can threaten their survival and long-term health.
- Low birth weight: Newborns can have low birth weight, leading to further health challenges.
- Preeclampsia: This dangerous rise in blood pressure during late pregnancy can affect major organs like the kidneys, liver, and heart.
- Placental abruption: Early separation of the placenta from the uterine wall before birth, causing complications for both mother and baby.
- Neurodevelopmental issues: Untreated hypothyroidism, especially, can lead to impaired brain development in the fetus, causing lower IQ and delayed motor and cognitive development in the child.
- Heart failure and thyroid storm: Severe, uncontrolled hyperthyroidism can lead to maternal heart failure and a life-threatening thyroid storm, which needs emergency treatment.
- Autoimmune thyroid problems in the baby: Babies can have thyroid enlargement (goiter) or thyroid dysfunction due to maternal antibodies crossing the placenta.
Regular monitoring and management by a specialist, such as the Best Infertility Specialist in Bhubaneswar, is crucial to minimize these risks and support healthy pregnancy outcomes.

Why is managing thyroid levels crucial for avoiding birth defects?
Managing thyroid levels during pregnancy is crucial to avoid birth defects because thyroid hormones play an essential role in the development of the fetal brain and nervous system, particularly in early pregnancy when the fetus depends entirely on maternal thyroid hormones. Inadequate thyroid hormone levels, especially due to hypothyroidism, can lead to irreversible effects like impaired cognitive development, lower IQ, and delayed neurological maturation in the child. Uncontrolled thyroid dysfunction increases risks, including miscarriage, premature birth, low birth weight, and developmental abnormalities that can manifest as neurodevelopmental disorders or physical birth defects.
In Bhubaneswar, as elsewhere, uncontrolled thyroid conditions during pregnancy can severely affect fetal growth and organ development, raising the chance of birth complications. Proper management—with regular testing, medication adjustments, and specialist care—is key to ensuring healthy fetal growth and minimizing these risks. Early diagnosis and treatment by a specialist, such as an infertility specialist in Bhubaneswar, helps protect both maternal health and fetal well-being.
To summarize the critical reasons:
- Maternal thyroid hormones are vital for fetal brain and organ development.
- Imbalances (hypo- or hyperthyroidism) increase the risk of miscarriage, premature birth, and low birth weight.
- Thyroid dysfunction can cause neurodevelopmental disorders or birth defects.
- Early and ongoing management reduces these risks and promotes healthy outcomes.
Therefore, managing thyroid levels carefully during pregnancy in Bhubaneswar is essential to avoid birth defects and ensure the best possible health for mother and baby.

How does maternal thyroid dysfunction increase neurodevelopmental disorder risks in children?
Maternal thyroid dysfunction during pregnancy—whether hypothyroidism (low thyroid hormone levels) or hyperthyroidism (excess thyroid hormone)—increases the risk of neurodevelopmental disorders in children through several biological mechanisms that impair fetal brain development:
- Thyroid hormones are critical for brain development: In early pregnancy, before the fetal thyroid is functional (about 12–14 weeks), the fetus depends entirely on maternal thyroid hormones, especially thyroxine (T4), for neurodevelopmental processes such as neuronal proliferation, migration, differentiation, and myelination. Deficiency or excess disrupts these processes.
- Impairment of neuronal migration and brain structure formation: Thyroid hormones regulate the production of proteins like Reelin needed for guiding neurons to their correct positions in brain areas, including the cerebellum, corpus callosum, and cerebral cortex, which are essential for motor and cognitive functions. Dysfunction leads to abnormal brain architecture and reduced brain volumes associated with cognitive impairments.
- Increased risk of neurodevelopmental disorders: Maternal thyroid dysfunction is consistently linked with heightened risks of Autism Spectrum Disorder (ASD), Intellectual Disability, Attention Deficit Hyperactivity Disorder (ADHD), and behavioral/emotional problems in offspring. For example, uncontrolled hypothyroidism and hyperthyroidism during pregnancy have been associated with roughly 2–3 times increased risk of ASD, with severity related to the duration and timing of thyroid imbalance.
- Dose and timing effects: The longer the maternal thyroid hormone imbalance persists during pregnancy (especially early gestation), the higher the risk of neurodevelopmental disorders in the child. Early pregnancy is a particularly vulnerable period due to critical brain developmental windows.
- Other associated mechanisms: Maternal thyroid dysfunction can also induce epigenetic changes, alter fetal immune development, and affect neuroinflammation, further contributing to abnormal brain development and later neurodevelopmental symptoms.
Treatment with levothyroxine or antithyroid medication during pregnancy can mitigate some risks, but the evidence on preventing neurodevelopmental disorders remains mixed, especially when treatment starts after the first trimester.
Tips to Control Thyroid During Pregnancy
Here are scientifically backed methods to manage the thyroid during pregnancy:
1. Regular Thyroid Function Tests
Get your TSH, Free T4, and sometimes T3 levels checked regularly. Monitoring helps in adjusting medications accordingly.
2. Medication Compliance
For hypothyroidism, doctors generally prescribe levothyroxine. For hyperthyroidism, antithyroid medications like propylthiouracil (PTU) are given in early pregnancy. Never stop or adjust your dose without consulting the Best Infertility Specialist in Bhubaneswar.
3. Follow an Iodine-Rich Diet
Iodine is vital for thyroid hormone production. Include:
- Dairy products
- Iodized salt
- Eggs
- Fish
But avoid overconsumption, as excess iodine can also cause thyroid dysfunction.
4. Avoid Goitrogens in Excess
Foods like cabbage, cauliflower, soy, and broccoli should be consumed in moderation, especially if you are hypothyroid, as they may interfere with thyroid function.
5. Manage Stress
Stress impacts the endocrine system. Incorporate yoga, meditation, or breathing exercises to keep stress in check.
6. Get Enough Selenium and Zinc
These nutrients support thyroid hormone metabolism. Include nuts (especially Brazil nuts), seeds, meat, and legumes in your diet.
7. Stay Physically Active
Engage in light to moderate exercise, as advised by your doctor, to regulate metabolism and hormone function.
When to Consult a Specialist?
If you:
- Have a known thyroid disorder
- Have a family history of thyroid disease
- Are you experiencing unusual fatigue, weight changes, or mood swings
- Have had difficulty conceiving
Then it’s time to consult the Best Infertility Specialist in Bhubaneswar for personalized guidance and safe thyroid management during pregnancy.

FAQ
1. Why is it important to control thyroid during pregnancy?
✅ Uncontrolled thyroid can lead to complications like miscarriage, preterm birth, low birth weight, and developmental issues in the baby. Managing thyroid ensures a healthy pregnancy for both mother and child.
2. How often should thyroid levels be checked during pregnancy?
✅ Thyroid levels should be checked in early pregnancy and then every 4–6 weeks or as advised by your doctor to ensure proper control.
3. Can I take thyroid medication while pregnant?
✅ Yes, thyroid medications like levothyroxine (for hypothyroidism) are safe during pregnancy when taken under medical supervision.
4. What foods help manage thyroid during pregnancy?
✅ Iodine-rich foods (dairy, eggs, fish), selenium (nuts, seeds), and zinc (meat, legumes) support thyroid health. Avoid excess goitrogens like soy and cabbage.
5. Who should I consult for thyroid-related pregnancy care?
✅ Consult an endocrinologist or the Best Infertility Specialist in Bhubaneswar, like Dr. Soumya Das, for expert evaluation and personalized treatment.
Conclusion
Proper management of the thyroid during pregnancy is essential for a smooth pregnancy and a healthy baby. Through regular monitoring, medication, diet, and lifestyle changes, you can keep your thyroid levels in check.
As the Best Infertility Specialist in Bhubaneswar, I emphasize the importance of early detection and timely intervention for women planning to conceive or already expecting. Always follow medical advice, and never self-medicate, especially during this delicate phase of life.
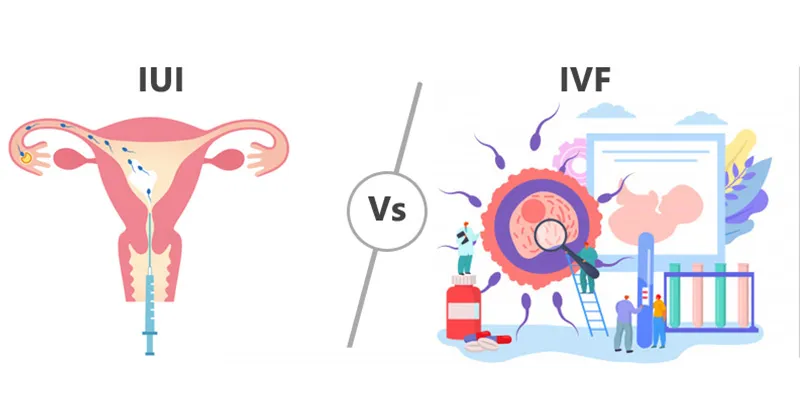
 t commonly searched causes of infertility today, with thousands of women asking online: “Can I get pregnant with endometriosis?” For many, the journey leads to IVF (In Vitro Fertilization)—a treatment that offers hope, but also raises important questions.
t commonly searched causes of infertility today, with thousands of women asking online: “Can I get pregnant with endometriosis?” For many, the journey leads to IVF (In Vitro Fertilization)—a treatment that offers hope, but also raises important questions.

 A miscarriage can be one of the most painful experiences in a couple’s fertility journey. Along with emotional grief, it often brings fear, confusion, and unanswered questions about the future. Many couples searching online ask the same question: “Can IVF help after a miscarriage?”
A miscarriage can be one of the most painful experiences in a couple’s fertility journey. Along with emotional grief, it often brings fear, confusion, and unanswered questions about the future. Many couples searching online ask the same question: “Can IVF help after a miscarriage?”