IVF is an emotionally, physically, and financially taxing experience. More often than one would like to think, it may not result in a positive pregnancy test. However, the fact is-IVF failure is more common than most people believe, and knowing exactly why it happens can enable you to make better decisions in your next cycle.
Following are the top 10 reasons for IVF failure and what you can do to improve your chances next time:
- Poor Egg Quality
A woman’s egg quality declines naturally with age, particularly after age 35. Poor-quality eggs may not fertilize properly or may result in abnormal embryos.
What You Can Do
- Discuss supplements like CoQ10 with your doctor
- Improve lifestyle habits: diet, sleep, and stress managemen
- Consider donor eggs, if advised.
- Poor Sperm Quality
A contributing factor to a large percentage of IVF failures is male infertility. Sperm count, motility, or morphological abnormalities can impact fertilization and subsequent embryo development.
What You Can Do
- Repeat a detailed semen analysis
- Lifestyle changes-smoking cessation, reduction in alcohol, and weight management
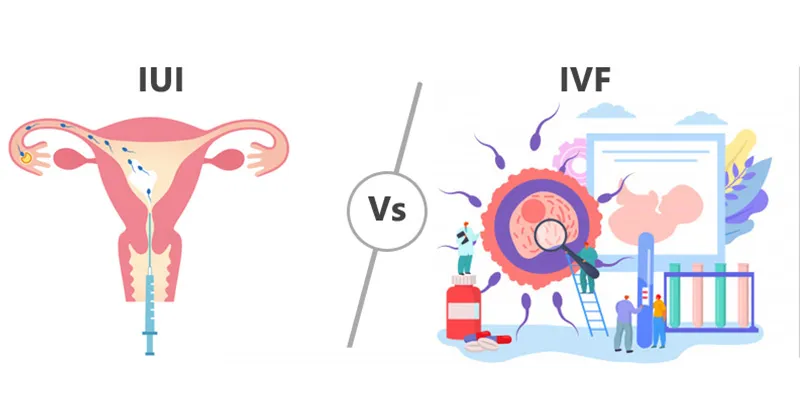
- Ask about ICSI (Intracytoplasmic Sperm Injection)
- Embryo Quality Issues
Not all embryos grow normally, even if the eggs and sperm look healthy. Genetic abnormalities, slow development, or poor grading can be the cause of implantation failure.
What You Can Do
- Consider PGT (Preimplantation Genetic Testing)
- Opt for the recommended blastocyst transfer
- Choose a clinic with advanced embryology labs
- Implantation Issues
Other times, an otherwise healthy embryo does not implant. This can be because of three things: lining problems in the uterus, poor blood flow, or hormonal imbalance.
What You Can Do
- Assess the endometrial thickness.
- Get tests for infections or inflammation
- Discuss ERA (Endometrial Receptivity Analysis) in case of repeated failures
- Uterine Abnormalities
Fibroids, polyps, a septum, or scar tissue are all contributing factors to poor embryo attachment and growth.
What You Can Do
- Undergo a hysteroscopy or ultrasound before the next cycle
- Treat fibroids or polyps
- Follow your doctor’s guidance concerning corrective procedures.
- Hormonal Imbalances
Proper levels of hormones support ovulation, the development of the oocyte, and uterine preparation. Thyroid, prolactin, estrogen, and progesterone imbalances may negatively impact IVF.
What You Can Do
- Get complete hormonal profiling
- Treat thyroid or prolactin problems
- Genetic Concerns
Sometime the cause is genetic—either in the egg, sperm, or embryo. These abnormalities can prevent embryos from forming or implanting.
What You Can Do
- Discuss genetic counseling
- Consider PGT-A or PGT-M testing
Use donor gametes if medically necessary
- Poor Ovarian Response
Some women, even with the use of stimulation injections, produce fewer eggs. This is often seen with low AMH or poor ovarian reserve.
What You Can Do
- Ask your doctor about modifying medication protocol
- discuss options such as mild stimulation IVF
- Consider egg donors in severe cases.
- Lifestyle Factors
Smoking, drinking, stress, obesity, lack of sleep, and poor diet influence the quality of the egg/sperm and chances of implantation.
What You Can Do
Follow a fertility-friendly diet
Maintain a healthy weight.
Get 7–8 hours of rest
Reduce stress through yoga, meditation, or counseling
ConnectionString Identifies the name of the database file that this web application will make use of.
- Laboratory or Technical Factors
IVF success also depends upon the technology and expertise of the clinic. Not all clinics have the same standards in their lab, equipment, or embryologist experience.
What You Can Do
- Choose a clinic with advanced embryology labs.
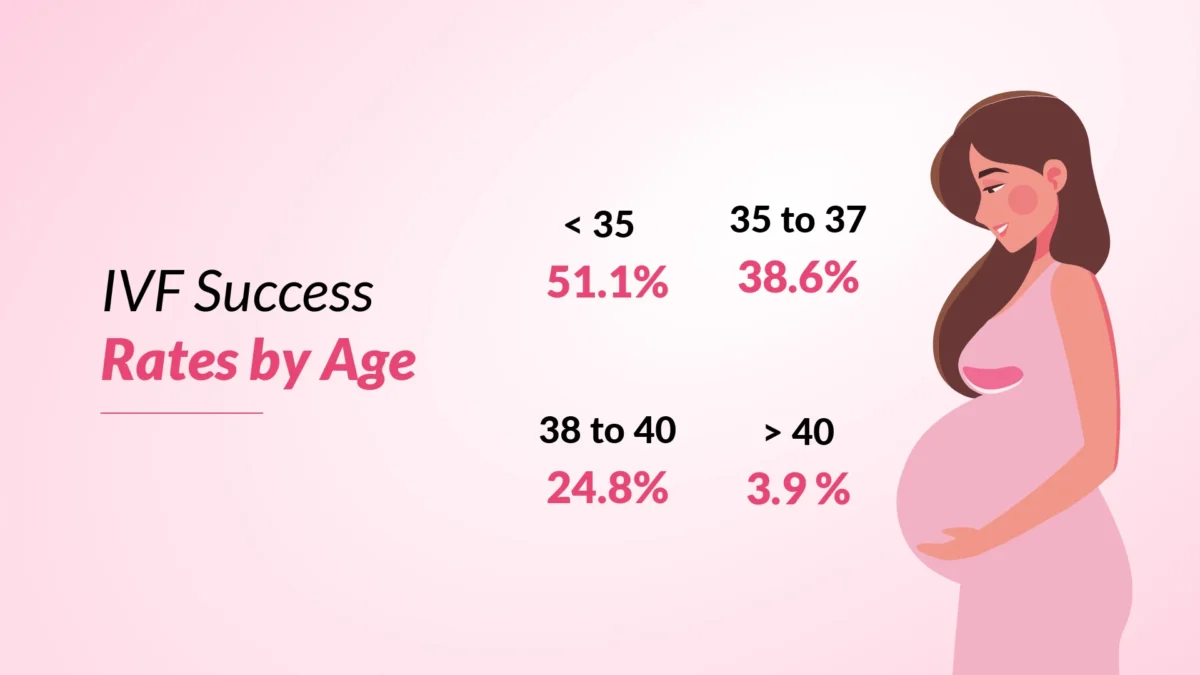
- Check success rates for your age group
- Ask about equipment, culture media, and protocols
What to Do After an IVF Failure: Your Action Plan
- Schedule a comprehensive follow-up consult
Discussion of reports, embryo grading, stimulation protocol, and possible reasons for failure.
- If necessary, request further tests
Clarity might also come from hormone tests, hysteroscopy, semen analysis, ERA, or genetic testing.
- Improve your lifestyle before the next cycle.
A 2–3 month gap with lifestyle optimization can significantly improve egg and sperm quality.
- Review of IVF protocol
Sometimes, a change in the medication protocol or a switch to FET (Frozen Embryo Transfer) improves success.
- Seek emotional support
IVF failure is considered a deeply stressful situation. Lean on your partner, friends, or support groups to heal emotionally.
- Seek a second opinion
Consulting another fertility specialist may be helpful if you have had more than one failed cycle.
Final Thoughts
Failure in IVF does not mark the end of your parenthood journey. Quite a number of couples succeed in getting pregnant once they understand the underlying causes and make necessary changes. With the right approach, proper medical support, and a healthy lifestyle, this next cycle will bring you closer to your dream of becoming parents.